Anterior Cervical Discectomy and Fusion
Anterior cervical discectomy and fusion (ACDF) is a surgical procedure used to treat a herniated or degenerated disc in the cervical spine, which is the upper part of the spine located in the neck.
Causes
Symptoms
Treatment
Causes
A herniated or degenerated disc in the cervical spine can be caused by a number of factors, including aging, wear and tear, and trauma.
Symptoms
The symptoms of a herniated or degenerated disc in the cervical spine can vary depending on the individual, but may include neck pain, arm pain, weakness or numbness in the arms or hands, and difficulty with fine motor skills.
Treatment
Non-surgical treatments such as physical therapy, medication, and injections are usually the first line of treatment for a herniated or degenerated disc in the cervical spine. However, if these treatments do not provide relief, ACDF may be recommended. During the procedure, the surgeon removes the damaged disc and replaces it with a bone graft or artificial disc to maintain stability in the spine.
Who needs it?
Anterior cervical discectomy and Fusion Operation operation is performed for two principal reasons, myelopathy and radiculopathy. In myelopathy, there is pressure on the spinal cord and the patient commonly experiences symptoms of stiffness and clumsiness in the hands and legs whereas in radiculopathy the nerve roots are under pressure or are inflamed causing symptoms of arm or shoulder pain and weakness. The two conditions not infrequently co-exist. If conservative management has failed to control the symptoms or if they are not at an acceptable level surgery may be indicated.
How is it done?
The operation is performed under general anaesthesia through a small incision at the front of the neck. The incision is usually placed in one of the skin creases, when feasible, and may typically be 2 – 3 cm in length. By parting the tissues in the neck the spine can easily be reached and the disc can be removed (having first confirmed that it is the correct disc using an x-ray. The surgeon may then use an operating microscope to better visualise the nerve roots at the back of the disc space to ensure that they are fully freed up.
Some surgeons do not attempt to achieve a fusion, but allow the disc space to heal up on its own, others will insert either a bone graft or cage (a metal one made from titanium, or a plastic one made of PEEK) into the disc space, to distract the disc space back to it’s normal height and to allow the fusion to occur in the best position. Dr Akbar Khan offers both options recommending what is best for patients.
What are the risks?
There are short term risks, arising at the time of surgery and long term risks occurring thereafter. Short term risks include damage to the spinal cord behind the damaged disc. This is said to be around a 1% risk per disc operated upon. The nerve roots behind the disc may potentially be damaged by the surgery or bleeding causing a build up of pressure. The structures in the neck including the trachea, oesophagus and blood vessels are at risk. There is a small nerve, the recurrent laryngeal nerve, which runs in the groove between the trachea and oesophagus, which if damaged, may lead to vocal cord paralysis on the affected side. This may require treatment from a throat specialist or may resolve spontaneously.
Putting all these risks together, including the general risk of anaesthesia and infection, the total is around 1 – 2%. The late risks include the possibility that the fusion will not heal, leading to a return of the pain the patient previously suffered, or that the bone graft will collapse, still fusing, but in a flexed posture. This latter is often prevented by inserting a metal plate over the bone graft.
Recovery
Most patients are out of bed on the morning after surgery, are generally given a soft collar to wear for comfort and are allowed home whenever they feel up to it, typically a day or so later. Arm pain caused by the nerve being trapped by the disc usually resolves completely and quickly (often within hours of the surgery). Neck pain, however, may be due to multiple causes including the bad disc and therefore, the results are less predictable.
X-rays are taken at six weeks post-operatively to ensure healing is occurring and may be repeated after a further six weeks.
Most patients are able to return to light work within two to three weeks but those in heavy manual labour will need to await bony fusion before returning, which may take three months.
Sports need to be avoided until healing has occurred, if these involve contact (soccer, rugby, etc.) but non-contact sport can be recommenced typically four weeks after surgery.
More Spinal Conditions

Spine Tumor Surgery in Karachi: Leading the Way with Prof. Dr. Akbar Ali Khan, Best Neurosurgeon in Pakistan

Advancing Spinal Health: Understanding Vertebrectomy with Prof. Dr. Akbar Ali Khan

Spinal Cord Stimulation

Kyphoplasty and Vertebroplasty
Vertebrectomy/Corpectomy

Foraminotomy
Cervical Disc Replacement

Anterior Cervical Discectomy and Fusion
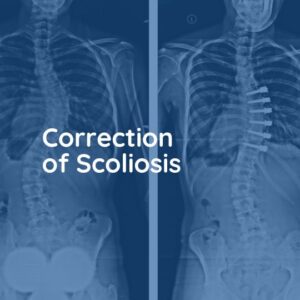
Correction of Scoliosis

Thoracic Discectomy

Lumbar Facet Joint Replacement

Interspinous Spacers

Endoscopic Lumbar Discectomy

Laminectomy

Disc Replacement Operation

Posterior Lumbar Fusion


